Heart Transplant
A heart transplant is a procedure in which a surgeon removes a diseased heart and replaces it with a donor heart. During a heart transplant, a mechanical pump circulates blood through the body while the surgeon removes the diseased heart and replaces it with a healthy heart from a recently deceased donor. The surgeon connects the donor heart to the major blood vessels and hooks the heart up to wires that temporarily control the heartbeat. The procedure takes several hours. To prevent the body from rejecting the donor heart, your surgeon will give you powerful drugs (immunosuppressants) right after surgery. You must continue to take them.
Heart transplant
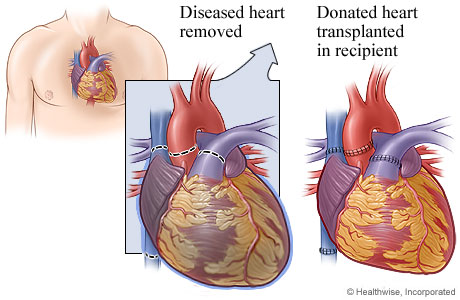
For a heart transplant, the diseased heart is removed and replaced with the donated heart. During the surgery, a mechanical pump moves blood through the body.
Why It's Done
Why is heart transplant surgery done?
A heart transplant is an option when the heart no longer works well enough and a person is at risk of dying. A heart transplant may be considered when a person has severe heart disease and is likely to benefit most from a donor heart. A person might be a candidate for a transplant when any of these conditions are true:
- The person has end-stage heart failure, ischemic heart disease, cardiomyopathy, or congenital heart disease.
- The person has a low chance of living as long as 1 year without a heart transplant.
- The person has no other serious medical conditions that would reduce life expectancy.
- The doctor strongly expects that a heart transplant will increase survival and improve the person's quality of life.
At some centers, transplant candidates must demonstrate that they have quit smoking and/or overusing alcohol for a period of time (such as 4 to 6 months) before they are considered for placement on a transplant waiting list.
Before Transplantation
How do you prepare for heart transplant surgery?
Surgery can be stressful. This information will help you understand what you can expect. And it will help you safely prepare for surgery.
Preparing for surgery
- Be sure you have someone to take you home. Anesthesia and pain medicine will make it unsafe for you to drive or get home on your own.
- Understand exactly what surgery is planned, along with the risks, benefits, and other options.
- If you take a medicine that prevents blood clots, your doctor may tell you to stop taking it before your surgery. Or your doctor may tell you to keep taking it. (These medicines include aspirin and other blood thinners.) Make sure that you understand exactly what your doctor wants you to do.
- Tell your doctor ALL the medicines, vitamins, supplements, and herbal remedies you take. Some may increase the risk of problems during your surgery. Your doctor will tell you if you should stop taking any of them before the surgery and how soon to do it.
- Make sure your doctor and the hospital have a copy of your advance directive. If you don’t have one, you may want to prepare one. It lets others know your health care wishes. It’s a good thing to have before any type of surgery or procedure.
Preparing for Heart Transplant
What happens on the day of your heart transplant surgery?
- Follow the instructions exactly about when to stop eating and drinking. If your doctor told you to take your medicines on the day of surgery, take them with only a sip of water.
- Take a bath or shower before you come in for your surgery. Do not apply lotions, perfumes, deodorants, or nail polish.
- Do not shave the surgical site yourself.
- Take off all jewelry and piercings. And take out contact lenses, if you wear them.
At the hospital or surgery center
- Bring a picture ID.
- You will be kept comfortable and safe by your anesthesia provider. You will be asleep during the surgery.
- The surgery will take at least 4 hours.
- You will go to the intensive care unit (ICU) right after surgery. You may stay in the ICU for 1 or 2 days before you go to your regular hospital room.
- You will have a breathing tube down your throat. This is usually removed within 6 hours after surgery. You will not be able to talk or drink liquids while the tube is in your throat. After the tube is removed, your throat will feel dry and scratchy. Your nurse will tell you when it is safe to drink liquids again.
- As you wake up in the ICU, the nurse will check to be sure you are stable and comfortable. It is important for you to tell your doctor and nurse how you feel and ask questions about any concerns you may have.
- You will have a thin plastic tube, called a catheter, in a vein in your neck. It is used to keep track of how well your heart is working. This is usually removed in 1 to 3 days.
- You will also have a catheter in an artery in your arm. It is used to check your blood pressure and take blood samples.
- You will have chest tubes to drain fluid and blood after surgery. The fluid and extra blood are normal and usually last only a few days. The chest tubes are usually removed in 1 or 2 days.
- You will have several thin wires coming out of your chest near your incision. These wires can help keep your heartbeat steady after surgery. They will be removed before you go home.
- You will have a tube that drains urine from your bladder. This is called a urinary catheter. It is usually removed within 1 day.
- You may have a thin plastic tube in your nose that goes down the back of your throat into your stomach. It will drain stomach juices. It is usually removed in the days after surgery.
Risks
What are the risks of heart transplant surgery?
Risks from heart transplant include:
- Rejection of the donor heart.
- To check for rejection, surgeons will regularly test a sample (biopsy) of the heart tissue. They'll also do echocardiography, electrocardiography (ECG, EKG), or blood tests.
- If your body rejects the heart, you will receive other drugs (such as immunosuppressants or steroids) to suppress your immune system so that it does not reject the donor heart. These drugs may have serious side effects, including an increased risk of infections and cancer.
- Infection.
- Clogging of the arteries (atherosclerosis) that may develop in the donor heart. (This is usually a complication and can affect long-term survival.)
- Death.
Your Recovery
Heart transplant: Your recovery
A heart transplant is surgery in which your diseased heart is replaced with a healthy donor heart. Your doctor did the surgery through a cut (incision) in your chest.
You will feel tired and sore for several weeks after surgery. You may have some brief, sharp pains on either side of your chest. Your chest, shoulders, and upper back may ache. The incision in your chest may be sore or swollen. These symptoms usually get better after 4 to 6 weeks.
You will probably be able to do many of your usual activities after about 3 months. But for 3 to 4 months, you will not be able to lift heavy objects or do activities that strain your chest or upper arm muscles. At first you may notice that you get tired easily and need to rest often. It may take several months to get your energy back.
Having an organ transplant can bring up many emotions. You may feel grateful and happy. But you also may feel guilty or depressed. Seek out family, friends, and counselors for support. If you think you are depressed, ask your doctor for help. Treatment can help you feel better.
After a heart transplant, you must follow a strict lifestyle involving daily medicines and regular medical care. This includes regular sampling (biopsies) of the transplanted heart tissue to check for rejection.
You probably started a cardiac rehabilitation (rehab) program in the hospital. You will continue with this rehab program after you go home to help you recover and prevent problems with your heart.
After Transplant: When To Call
After a heart transplant: When to call
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have severe trouble breathing.
- You have sudden chest pain and shortness of breath, or you cough up blood.
- You have severe pain in your chest.
- You have symptoms of a stroke. These may include:
- Sudden numbness, tingling, weakness, or loss of movement in your face, arm, or leg, especially on only one side of your body.
- Sudden vision changes.
- Sudden trouble speaking.
- Sudden confusion or trouble understanding simple statements.
- Sudden problems with walking or balance.
- A sudden, severe headache that is different from past headaches.
- You have symptoms of a heart attack. These may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly or in one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
Call your doctor now or seek immediate medical care if:
- You have pain that does not get better after you take pain medicine.
- You have loose stitches, or your incision comes open.
- You are bleeding a lot from the incision.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
- You have signs of a blood clot, such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness and swelling in your leg or groin.
- Your heartbeat feels very fast, skips beats, or flutters.
- You have symptoms of heart failure, such as:
- Swelling in your legs, ankles, or feet.
- Sudden weight gain, such as more than 2 to 3 pounds in a day or 5 pounds in a week. (Your doctor may suggest a different range of weight gain.)
- You are sick to your stomach or cannot keep fluids down.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You do not get better as expected.
Self-Care
How can you care for yourself after a heart transplant?
Activity
Continue the cardiac rehab program you started in the hospital. Your program has details about your activity level and your diet. Here are some general guidelines:
- Rest when you feel tired. Getting enough sleep will help you recover. Try to sleep on your back while your breastbone (sternum) heals. This usually takes about 4 to 6 weeks.
- Try to walk each day as directed by your cardiac rehab program. Start by walking a little more than you did the day before. Bit by bit, increase the amount you walk. Walking boosts blood flow and helps prevent pneumonia and constipation.
- Avoid strenuous activities, such as bicycle riding, jogging, weight lifting, or heavy aerobic exercise, until your doctor says it is okay.
- For 3 months, avoid activities that strain your chest or upper arm muscles. This includes pushing a lawn mower or vacuum, mopping floors, or swinging a golf club or tennis racquet.
- For at least 6 weeks, avoid lifting anything that would make you strain. This may include heavy grocery bags and milk containers, a heavy briefcase or backpack, cat litter or dog food bags, or a child.
- For at least 6 weeks, avoid pushing yourself up out of a bed or chair using your arms. Do not use your arms to pull yourself into or out of a vehicle.
- Hold a pillow firmly over your chest incision when you cough or take deep breaths. This will support your chest and reduce your pain.
- Do breathing exercises at home as instructed by your doctor. This will help prevent pneumonia.
- Ask your doctor when you can drive again.
- You may need to take 4 to 12 weeks off from work. It depends on the type of work you do and how you feel.
- Ask your doctor when it is okay for you to have sex.
Diet
- Eat a heart-healthy diet. If you have not been eating this way, talk to your doctor. You also may want to talk to a dietitian. A dietitian can help you plan meals and learn about healthy foods.
- Drink plenty of fluids (unless your doctor tells you not to).
- You may notice that your bowel movements are not regular right after your surgery. This is common. Try to avoid constipation and straining with bowel movements. You may want to take a fiber supplement every day. If you have not had a bowel movement after a couple of days, ask your doctor about taking a mild laxative.
Medicines
- Your doctor will tell you if and when you can restart your medicines. You will also be given instructions about taking any new medicines.
- If you stopped taking aspirin or some other blood thinner, your doctor will tell you when to start taking it again.
- Be safe with medicines. Your doctor will give you anti-rejection medicines. Your doctor may also give you medicines to prevent blood clots, keep your heartbeat steady, and lower your blood pressure and cholesterol. Take your medicines exactly as prescribed. Call your doctor if you think you are having a problem with your medicine.
- Take pain medicines exactly as directed.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- Do not take aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), or other nonsteroidal anti-inflammatory drugs (NSAIDs) unless your doctor says it is okay.
- If you think your pain medicine is making you sick to your stomach:
- Take your medicine after meals (unless your doctor has told you not to).
- Ask your doctor for a different pain medicine.
- If your doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
- Your doctor may give you a blood thinner to prevent blood clots. If you take a blood thinner, be sure you get instructions about how to take your medicine safely. Blood thinners can cause serious bleeding problems.
Incision care
- If you have strips of tape on the cuts (incisions) the doctor made, leave the tape on for a week or until it falls off.
- Wash the area daily with warm, soapy water, and pat it dry. Don't use hydrogen peroxide or alcohol, which can slow healing. You may cover the area with a gauze bandage if it weeps or rubs against clothing. Change the bandage every day.
- You can take showers with your back to the showerhead. Allow the warm and soapy water to run across your shoulders and down over the incision. Pat the incision dry with a clean towel.
- Do not take a bath for the first 3 weeks, or until your doctor tells you it is okay.
- Do not swim or use a hot tub for at least 1 month, or until your doctor says it is okay.
- Do not use any creams, lotions, powders, ointments, or oils unless your doctor tells you it is okay.
Other instructions
- Keep track of your weight. Weigh yourself every day at the same time of day, on the same scale, in the same amount of clothing. A sudden increase in weight can be a sign of a problem with your heart. Tell your doctor if you suddenly gain weight, such as 3 pounds or more in 2 to 3 days.
Copyrighted material adapted with permission from Healthwise, Incorporated. This information does not replace the advice of a doctor.




