Varicose Veins
Overview
Varicose veins are twisted, enlarged veins near the surface of the skin. They develop most often in the legs and ankles.
Some people may be more likely than others to get varicose veins because of aging or hormone changes or because a parent has them. Being overweight or pregnant can make varicose veins worse. Jobs that require standing for long periods of time also can make them worse.
Symptoms
Varicose veins
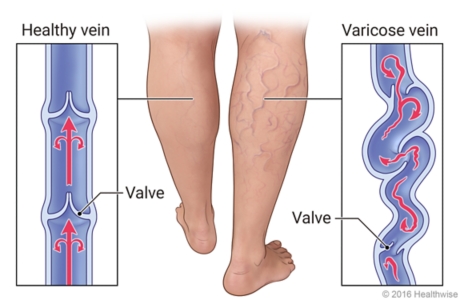
Varicose veins are caused by weakened valves and veins in your legs. Normally, one-way valves in your veins keep blood flowing from your legs up toward your heart. When these valves don't work as they should, blood collects in your legs, and pressure builds up. The veins become weak, large, and twisted.
What are the symptoms of varicose veins?
Varicose veins look like swollen and twisted blood vessels under the skin. They may not cause any symptoms. Mild symptoms may include:
- Heaviness, burning, aching, tiredness, or pain in your legs. These symptoms may be worse after you stand or sit for long periods of time.
- Mild swelling in your feet and ankles.
- Itching over the vein.
More serious symptoms include:
- Leg swelling.
- Swelling and calf pain after you sit or stand for long periods of time.
- Skin changes, such as:
- Color changes.
- Dry, thinned skin.
- Inflammation.
- Scaling.
- Open sores.
- Bleeding after a minor injury.
- Superficial thrombophlebitis. This happens when a blood clot and inflammation form in a small vein near the surface of the skin.
Causes
What causes varicose veins?
Varicose veins are caused by weakened valves and veins in your legs. Normally, one-way valves in your veins keep blood flowing from your legs up toward your heart. When these valves don't work as they should, blood collects in your legs, and pressure builds up. The veins become weak, large, and twisted.
Varicose veins often run in families. You may be born with defective valves or weak walls in your veins, or you may develop them later in life. Varicose veins happen more often as people get older.
Varicose veins often form during pregnancy. They might become less prominent after pregnancy and may disappear completely.
Prevention
Preventing varicose veins
Varicose veins may be prevented to some extent. Here are a few things you can try.
- Stay at a healthy weight.
Lose weight if you need to.
- Get regular exercise.
Exercise may help improve blood flow in your legs.
- Avoid long periods of standing or sitting.
- Avoid crossing your legs at the knee while sitting.
- Do not smoke.
Diagnosis
How are varicose veins diagnosed?
Varicose veins are most often diagnosed based on how they look. No special tests are needed to confirm the diagnosis.
Your doctor will:
- Ask questions about any risk factors, such as vein problems, serious leg injuries, or leg ulcers you've had in the past.
- Do a physical exam. The doctor will examine your legs and feet (or any other affected areas). The doctor will check for tender areas, swelling, skin color changes, ulcers, and other signs of skin breakdown.
You might need tests if you plan to have treatment or if you have signs of a deep vein problem. Duplex Doppler ultrasound is the most commonly used test. It can help your doctor study blood flow in your leg veins.
Treatment
How are varicose veins treated?
The goals of treatment for varicose veins are to reduce symptoms and prevent complications. For some, the goal may be related to how the veins look. Home treatment is usually the first approach.
Home treatment
Home treatment may be all you need to ease your symptoms and keep the varicose veins from getting worse. You can:
- Wear compression stockings.
- Stay at a healthy weight.
- Prop up (elevate) your legs.
- Avoid long periods of sitting or standing.
- Get regular exercise.
Procedures
If home treatment doesn't help, there are procedures that can treat varicose veins. These include:
- Endovenous ablation.
-
Endovenous ablation is a procedure to close off varicose veins. Endovenous means that the procedure is done inside the vein. Ablation means a doctor uses something to damage and close off the vein. This may be heat, chemicals, or a small wire.
- Ligation and stripping.
This treatment is a type of surgery. Cuts (incisions) are made over the varicose vein, and the vein is tied off (ligated) and removed (stripped).
- Phlebectomy.
Several tiny cuts are made in the skin through which the varicose vein is removed. This is also called microphlebectomy, ambulatory phlebectomy, or stab avulsion.
- Sclerotherapy.
A chemical is injected into a varicose vein to damage and scar the inside lining of the vein, causing the vein to close.
- Simple laser treatment.
-
Laser energy is used to scar and destroy varicose veins. Simple laser therapy is done on small veins close to the skin, such as spider veins. The laser is used outside of your skin.
The size of your varicose veins affects your treatment options.
- Larger varicose veins are generally treated with endovenous ablation or ligation and stripping surgery.
- Smaller varicose veins and spider veins are usually treated with sclerotherapy or simple laser therapy on your skin.
When to Call
Varicose veins: When to call
Call 911 anytime you think you may need emergency care. For example, call if:
- You have sudden chest pain and shortness of breath, or you cough up blood.
Call your doctor now or seek immediate medical care if:
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Swelling in the leg or groin.
- A color change on the leg or groin. The skin may be reddish or purplish, depending on your usual skin color.
- A varicose vein begins to bleed and you cannot stop it.
- You have a tender lump in your leg.
- You get an open sore.
Watch closely for changes in your health, and be sure to contact your doctor if:
- Your varicose vein symptoms do not improve with home treatment.
Self-Care
How can you care for yourself when you have varicose veins?
- Wear compression stockings during the day to help relieve symptoms and improve blood flow. Talk to your doctor about which ones to get and where to get them.
- Prop up your legs at or above the level of your heart when possible. Try to do this for about 30 minutes at a time, about 3 times a day. This helps keep the blood from pooling in your lower legs and improves blood flow to the rest of your body.
- Avoid sitting and standing for long periods. This puts added stress on your veins.
- Stay at a healthy weight. Lose weight if you need to.
- Try to take several short walks every day.
- Get at least 30 minutes of exercise on most days of the week. Walking is a good choice. You also may want to do other activities, such as running, swimming, cycling, or playing tennis or team sports.
- Do calf muscle exercises every day. When you are sitting down, rotate your feet at the ankles in both directions, making small circles. Extend your legs, and point and flex your feet.
- Avoid crossing your legs at the knees when sitting.
- Take good care of your skin. Treat cuts and scrapes on your legs right away. Keep your legs clean and moisturized to prevent drying and cracking. Prevent sunburns.
- Do not smoke. Smoking can make varicose veins worse. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- If you bump your leg so hard that you know it is likely to bruise, prop up your leg and apply ice or cold packs right away. Apply the ice or cold pack for 10 to 20 minutes, 3 or more times a day. Put a thin cloth between the ice and your skin.
- If you cut or scratch the skin over a vein, it may bleed a lot. Prop up your leg and apply firm pressure for a full 15 minutes.
If you have a blood clot in a varicose vein, you may have tenderness and swelling over the vein. The vein may feel firm. Be sure to call your doctor right away if you have these symptoms. If your doctor has told you how to care for the clot, follow the instructions. Care may include the following:
- Prop up your leg and apply a damp cloth that is warm or cool.
- Ask your doctor if you can take an over-the-counter pain medicine, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve). Be safe with medicines. Read and follow all instructions on the label.
Copyrighted material adapted with permission from Healthwise, Incorporated. This information does not replace the advice of a doctor.


