Heartburn
Heartburn is an uncomfortable feeling or burning pain behind the breastbone. It may occur after eating, soon after lying down, when bending forward, or after taking certain medicines.
Heartburn occurs when stomach acid backs up (refluxes) into the tube that leads from the mouth to the stomach (esophagus), causing pain or discomfort behind the breastbone, in the center of the chest, and occasionally in the back of the throat. Sometimes there may be a sour or bitter taste in the mouth.
Antacids or other nonprescription medicines (such as acid reducers or acid blockers) may relieve heartburn.
Heartburn can be a symptom of gastroesophageal reflux disease (GERD).
Symptoms
Heartburn
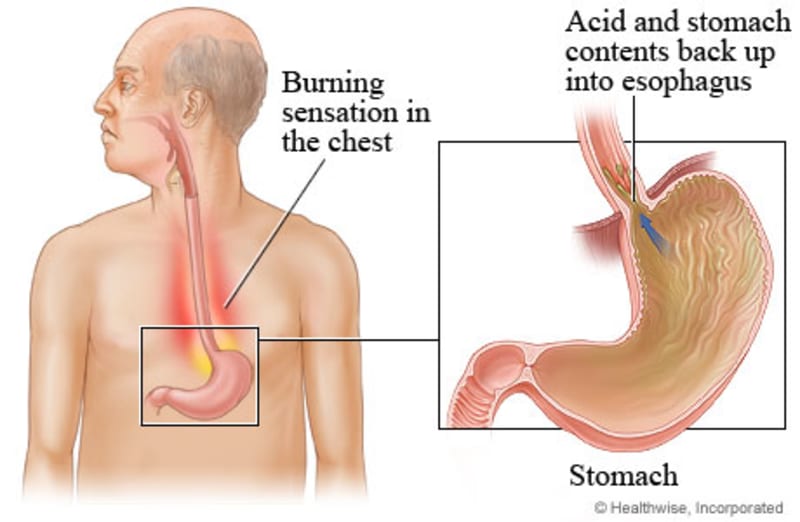
Heartburn is a feeling of burning, warmth, heat, or pain that often starts in the upper abdomen just beneath the lower breastbone (sternum). This discomfort may spread in waves upward into your throat, and you may have a sour taste in your mouth.
Controlling heartburn
Changing your habits to control heartburn from gastroesophageal reflux disease (GERD)
Symptoms of GERD can be painful and, if allowed to continue, can lead to complications including esophagitis. Esophagitis is irritation or inflammation of the esophagus.
You can make changes to your lifestyle to help relieve your symptoms of GERD. Here are some things to try.
- Stay at a weight that's healthy for you.Extra weight puts more pressure on your stomach and makes you more likely to have heartburn. Losing even a few pounds can help. Talk to your doctor if you need help losing weight.
- Change your eating habits.Try to eat several small meals instead of two or three large meals. After you eat, wait 2 to 3 hours before you lie down. Snacking close to bedtime can make your symptoms worse. Avoid foods that make your symptoms worse. These may include chocolate, mint, alcohol, pepper, spicy foods, high-fat foods, or drinks with caffeine in them, such as tea, coffee, colas, or energy drinks. If your symptoms are worse after you eat a certain food, you may want to stop eating that food to see if your symptoms get better.
- Try to quit smoking or chewing tobacco, or cut back as much as you can.If you need help quitting, talk to your doctor about quit-tobacco programs and medicines. These can increase your chances of quitting for good.
- Raise your bed if you have GERD symptoms when you are trying to sleep.Put the frame on blocks or place a foam wedge under the head of your mattress to raise the head of your bed 6 in. (15 cm) to 8 in. (20 cm). Adding extra pillows does not work.
- Avoid or reduce pressure on your stomach.Don't wear tight clothing around your middle.
Changing your sleep habits to control heartburn from gastroesophageal reflux disease (GERD)
Here are some things you can try.
- Raise the head of your bed 6 in. (15 cm) to 8 in. (20 cm).
This will help keep stomach acid from flowing into your esophagus when you are sleeping.
You can do this by putting blocks underneath your bed frame or by placing a foam wedge under the head of your mattress. Using extra pillows will not work.
- Wait 2 to 3 hours after you eat before you lie down.
Lying down soon after eating will also increase the chance of getting heartburn.
Snacking close to bedtime can make your symptoms worse.
Quitting tobacco to control heartburn from gastroesophageal reflux disease (GERD)
If you smoke or chew tobacco, try to quit or cut back. The nicotine from tobacco relaxes the valve between the esophagus and stomach (lower esophageal sphincter). This can allow stomach acid and juices, the chemicals that break down food in the stomach, to back up (reflux) into the esophagus, which can cause heartburn.
Because the nicotine in tobacco is addicting, stopping the use of tobacco is more difficult than simply changing a habit. Those who successfully quit using tobacco usually use a combination of these strategies.
- Seek professional counseling, either by telephone or in person.
- Use medicines to help overcome the addiction to nicotine.
- Participate in a proven smoking cessation program.
- Join a support group of peers who are also quitting or who do not smoke.
Reducing pressure on your stomach to control heartburn from gastroesophageal reflux disease (GERD)
Putting pressure on your stomach may push stomach juices into your esophagus, causing heartburn. Here are some things you can try.
- Wait 2 to 3 hours after you eat before you lie down.
When you are lying down, the contents of your stomach can push against the valve between the esophagus and stomach (lower esophageal sphincter).
Sitting up allows gravity to help food and stomach juices from the esophagus drain back into your stomach.
Snacking close to bedtime can make your symptoms worse.
- Avoid tight clothing over your stomach.
Tight belts, waistbands, or panty hose may push against your stomach and make your heartburn worse.
- Use care when lifting and bending.
Bending over tends to increase the amount of stomach acid that can get into your esophagus.
When lifting, bend your knees to avoid bending over at the waist.
Treatment
Nonprescription antacids: Overview
Many people take nonprescription antacids for mild or occasional heartburn. Antacids are substances that neutralize some of the stomach acid.
Examples of nonprescription antacids include:
- Rolaids.
- Maalox.
- Mylanta.
- Tums.
Be careful when you take over-the-counter antacid medicines. Many of these medicines have aspirin in them. Read the label to make sure that you are not taking more than the recommended dose. Too much aspirin can be harmful. If you are pregnant, do not take aspirin or medicines that contain aspirin unless your doctor says it is okay.
Some nonprescription antacids are safe to use during pregnancy to treat heartburn symptoms. Antacids that contain sodium bicarbonate should not be taken during pregnancy because they can cause fluid buildup. And do not use antacids that have magnesium trisilicate, because they may not be safe for your baby.
If you need to use antacids frequently, talk with your doctor or pharmacist about their recommendations and cautions. Be sure to follow the package directions.
Self-care
How can you care for yourself when you have heartburn?
Home treatment, such as lifestyle changes and nonprescription medicines, may be all that's needed to treat heartburn. But if your symptoms don't get better with home treatment, or if your symptoms occur often, there may be other medical problems causing your symptoms.
Keep a record of your heartburn symptoms before and after you make lifestyle changes or use nonprescription medicines so you can track any improvement or changes.
Medicines to treat heartburn
The two main types of medicines for heartburn are antacids and stomach acid reducers.
Antacids
Many people take nonprescription antacids for mild or occasional heartburn.
- Antacids such as Tums, Mylanta, or Maalox neutralize some of the stomach acid. They work for 30 minutes to 2 hours, depending on whether the stomach is full or empty. Liquid or dissolving antacids usually work faster than tablet forms.
- Antacids such as Pepto-Bismol coat the esophagus and act as a barrier to reflux acid. Pepto-Bismol should not be used for more than 3 weeks. And you shouldn't take it if you can't take aspirin. It may make your tongue or stools black. The black color usually isn't serious. Brushing your teeth and tongue after you take Pepto-Bismol may keep your tongue from turning black.
Antacids work faster than acid reducers (H2 blockers). But their effect doesn't last more than 1 to 2 hours. H2 blockers can provide relief for up to 12 hours.
Antacids have side effects. They may cause diarrhea or constipation. And they can interfere with how your body absorbs other medicines.
Be careful when you take over-the-counter antacids. Many of these medicines have aspirin in them. Read the label to make sure that you aren't taking more than the recommended dose. Too much aspirin can be harmful.
Stomach acid reducers
- H2 blockers.
-
Histamine receptor (or H2) blockers decrease the amount of acid that the stomach makes. This may reduce irritation of the stomach lining and decrease heartburn. Some examples of nonprescription acid reducers are cimetidine (Tagamet HB) and famotidine (Pepcid AC).
- Proton pump inhibitors.
-
Proton pump inhibitors (PPIs), such as omeprazole (for example, Prilosec), reduce stomach acid. These acid-reducing medicines are used when your heartburn hasn't gotten better with other home treatments, antacids, or H2 blockers. You may need to use a PPI for up to 5 days before you have relief of your heartburn. You can buy PPIs without a prescription.
Cautions
- If you are pregnant and have heartburn symptoms, be sure to talk to your doctor before you take any heartburn medicines. Some medicines may not be safe to take while you are pregnant.
- If you use antacids more than just once in a while, talk with your doctor. If you have any health risks, be sure to talk with your doctor before you start to take an antacid. If you have kidney disease, it's even more important to discuss antacid use with your doctor. Regular use of antacids that contain magnesium or aluminum can cause a dangerous buildup of these two substances in people who have kidney disease.
- Talk with your doctor if you take an H2 blocker for more than 2 weeks.
- Acid reducers can sometimes change the way other medicines work. If you take prescription medicines, be sure to talk with your doctor before you take a nonprescription acid reducer.
Copyrighted material adapted with permission from Healthwise, Incorporated. This information does not replace the advice of a doctor.
